Stress incontinence occurs when the muscles and tissues that support the bladder and urethra become weakened or damaged. Pelvic floor dysfunction, childbirth, hormonal changes during menopause or pregnancy, and even obesity can increase your risk of developing this condition.
Treatment options for stress incontinence range from lifestyle modifications and exercises like Kegels to surgical procedures such as sling procedures and urethral bulking agents. The best approach for you will depend on the severity of your symptoms, the underlying cause of your incontinence, and your preferences.
Stress incontinence is characterized by involuntary urine leakage during physical activities that put pressure on the bladder. This can include coughing, sneezing, laughing, lifting heavy objects, physical activity, and high-impact exercises like running and jumping. The following are some common symptoms of stress incontinence:
The causes of stress incontinence can vary, but pelvic floor dysfunction is a common underlying factor. This dysfunction can be caused by pregnancy, childbirth, menopause, and aging. Women with vaginal deliveries or C-sections are at an increased risk of developing stress incontinence.
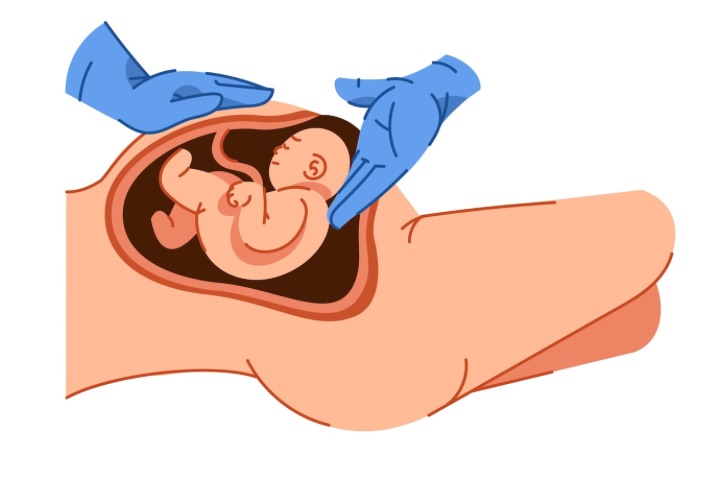
Photo Credit: Freepik
While stress incontinence can be a distressing and embarrassing condition, various treatment options and management strategies are available to help individuals cope with this issue and improve their quality of life.
Stress incontinence can be treated with a variety of approaches.
One of the most effective treatments for stress incontinence is to perform exercises that strengthen the pelvic floor muscles. Kegel exercises are the most common, which involve contracting and relaxing the muscles that control bladder function. Biofeedback therapy and electrical stimulation can also be used to help individuals better locate and target these muscles during exercise.
In some cases, surgery may be necessary to treat severe stress incontinence. Sling procedures involve placing a strip of material under the urethra to provide support and prevent urine leakage. Urethral bulking agents may also be injected around the urethra to add bulk and prevent leakage.
Pessaries are devices that are inserted into the vagina to provide support to the bladder or urethra. They can be used to help individuals with stress incontinence manage their symptoms without surgery or medication.
It is important to discuss the pros and cons of each treatment option with a healthcare provider to determine the best approach based on an individual’s specific needs and circumstances.
There are numerous ways to manage and treat stress incontinence, ranging from non-invasive solutions such as exercises and lifestyle modifications, to more invasive procedures like surgery. Treatment options will usually depend on the severity of the incontinence, the individual women’s health, and personal preference.

Photo Credit: Kues1
Simple lifestyle modifications can go a long way in managing stress incontinence. Maintaining a healthy weight, quitting smoking, and reducing your intake of caffeine and alcohol can all help. Additionally, avoiding constipation and following a regular exercise routine can also improve bladder control.
Kegel exercises, which involve contracting and relaxing the pelvic floor muscles, can help strengthen the muscles responsible for bladder control. Biofeedback therapy and electrical stimulation can be used to aid in the performance of these exercises. Physical therapy focusing on the pelvic floor can also be effective in treating stress incontinence.
Surgery may be required if your stress incontinence is severe and non-invasive treatments have not been successful. Procedures such as sling procedures, in which a sling is placed under the urethra to support it, and urethral bulking agents, which work to bulk up the urethra and prevent leakage, may be recommended.
It is important to discuss the potential risks and benefits of any surgical procedure with your healthcare provider before making a decision.
A pessary is a device that is inserted into the vagina to support the bladder and improve bladder control. This non-invasive solution can be effective in managing stress incontinence.
Combining different treatment methods, such as exercises and medication, can effectively manage stress incontinence. Your healthcare provider can help determine the best course of action based on your individual needs.
Various treatment options are available for managing and treating stress incontinence, from non-invasive solutions to surgical procedures. It is important to discuss all available options with your healthcare provider to determine which approach is best for you.

Photo Credit: Freepik
If you are struggling with stress incontinence, there are a variety of treatment options that may help improve your symptoms. Here are some of the most common:
One of the most effective ways to manage stress incontinence is to strengthen your pelvic floor muscles. Kegel exercises, in which you contract and release these muscles, can be done almost anywhere and can help reduce leakage. Other types of physical therapy, such as biofeedback therapy and electrical stimulation, can also help with muscle strengthening.
A pessary is a small, flexible device that is inserted into the vagina to help support the bladder and reduce leakage. There are different types of pessaries, such as those made of silicone or latex, and a healthcare provider can fit them.
In more severe cases of stress incontinence, surgery may be necessary. One common procedure is called a sling procedure, in which a mesh sling is placed under the urethra to provide support. Another option is the injection of a bulking agent into the tissue around the urethra to help keep it closed.
As with any surgery, there are risks and potential side effects associated with these procedures, so it is important to discuss all options with your healthcare provider.
The main cause of stress incontinence is the weakening or damage to the muscles and tissues that support the bladder and urethra, often due to factors such as childbirth, aging, or certain medical conditions.
Stress incontinence can be treated through various methods, including pelvic floor exercises (Kegel exercises), lifestyle changes, behavioral therapies, and in some cases, surgery.
The most common symptoms of stress incontinence include leakage of urine during physical activities such as coughing, sneezing, laughing, lifting, or exercising.
Mild stress incontinence can sometimes improve or go away with conservative treatments like pelvic floor exercises. However, severe cases may require more comprehensive treatment approaches or surgical intervention for better management. Consulting a healthcare professional is essential for personalised advice and treatment options.